Bronchiectasis
INTRODUCTION
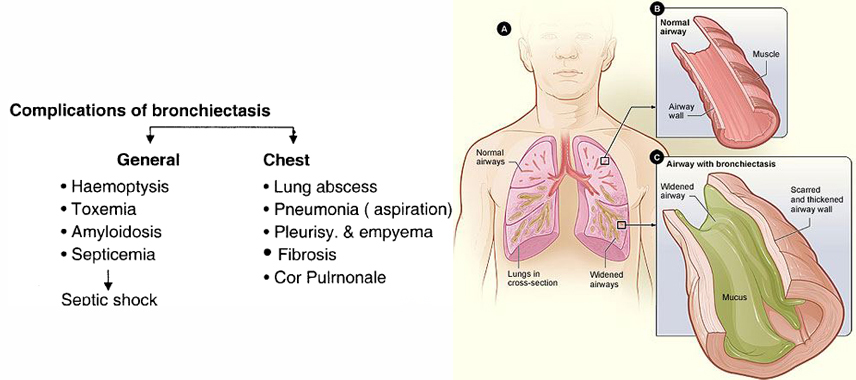
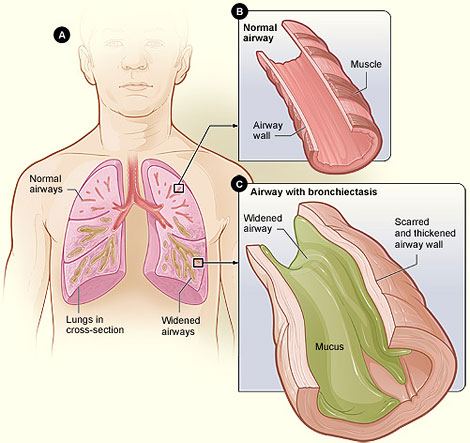
Bronchiectasis is a condition in which damage to the airways causes them to widen and become flabby and scarred. The airways are tubes that carry air in and out of your lungs.
Bronchiectasis often is caused by an infection or other condition that injures the walls of the airways or prevents the airways from clearing mucus. Mucus is a slimy substance. It helps remove inhaled dust, bacteria, and other small particles from the airways. In bronchiectasis, your airways slowly lose their ability to clear out mucus. The mucus builds up, and bacteria begin to grow. This leads to repeated, serious lung infections.
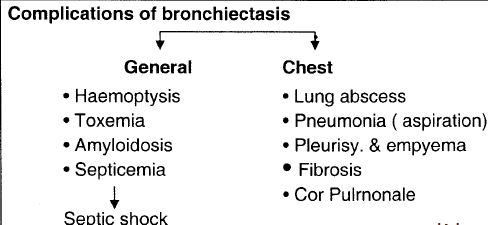
Each infection causes more damage to the airways. Over time, the airways can't properly move air in and out of the lungs. As a result, the body's vital organs might not get enough oxygen. Bronchiectasis can lead to serious health problems, such as respiratory failure, atelectasis and heart failure.
Bronchiectasis can affect just one section of one of your lungs or many sections of both lungs. The initial lung damage that leads to bronchiectasis often begins in childhood. However, symptoms may not occur until months or even years after you start having repeated lung infections.
WHAT CAUSES BRONCHIECTASIS?
Damage to the walls of the airways usually is the cause of bronchiectasis. A lung infection may cause this damage. Examples of lung infections that can lead to bronchiectasis include:
• Severe pneumonia
• Whooping cough or measles (uncommon in the United States due to vaccination)
• Tuberculosis
• Fungal infections
Conditions that damage the airways and raise the risk of lung infections also can lead to bronchiectasis. Examples of such conditions include:
• Cystic fibrosis. This disease leads to almost half of the cases of bronchiectasis in the United States.
• Immunodeficiency disorders, such as common variable immunodeficiency and, less often, HIV and AIDS.
• Allergic bronchopulmonary aspergillosis. This is an allergic reaction to a fungus called aspergillus. The reaction causes swelling in the airways.
• Disorders that affect cilia function, such as primary ciliary dyskinesia. Cilia are small, hair-like structures that line your airways. They help clear mucus (a slimy substance) out of your airways.
• Chronic (ongoing) pulmonary aspiration. This is a condition in which you inhale food, liquids, saliva, or vomited stomach contents into your lungs. Aspiration can inflame the airways, which can lead to bronchiectasis.
• Connective tissue diseases, such as rheumatoid arthritis, Sjögren’s syndrome, and Crohn’s disease.
Other conditions, such as an airway blockage, also can lead to bronchiectasis. Many things can cause a blockage, such as a growth or a noncancerous tumor. An inhaled object, such as a piece of a toy or a peanut that you inhaled as a child, also can cause an airway blockage.
A problem with how the lungs form in a fetus may cause congenital bronchiectasis. This condition affects infants and children.
SIGNS AND SYMTOMS
Some people with bronchiectasis may produce frequent green/yellow sputum (up to 240ml (8 oz) daily). Bronchiectasis may also present with coughing up blood in the absence of sputum, called "dry bronchiectasis". Sputum production may also occur without coloration. People with bronchiectasis may have bad breath indicative of active infection. Frequent bronchial infections and breathlessness are two possible indicators of bronchiectasis. Crepitations and expiratory rhonchi may be heard on auscultation, although nail clubbing is rare.
HOW IS BRONCHIECTASIS DIAGNOSED?
Your doctor may suspect bronchiectasis if you have a daily cough that produces large amounts of sputum (spit).
To find out whether you have bronchiectasis, your doctor may recommend tests to:
• Identify any underlying causes that require treatment
• Rule out other causes of your symptoms
• Find out how much your airways are damaged
Diagnostic Tests and Procedures
Chest CT scan
A chest computed tomography (to-MOG-ra-fee) scan, or chest CT scan, is the most common test for diagnosing bronchiectasis.
This painless test creates precise pictures of your airways and other structures in your chest. A chest CT scan can show the extent and location of lung damage. This test gives more detailed pictures than a standard chest x ray.
Chest x ray
This painless test creates pictures of the structures in your chest, such as your heart and lungs. A chest x ray can show areas of abnormal lung and thickened, irregular airway walls.
Other Tests
Your doctor may recommend other tests, such as:
• Blood tests. These tests can show whether you have an underlying condition that can lead to bronchiectasis. Blood tests also can show whether you have an infection or low levels of certain infection-fighting blood cells.
• A sputum culture. Lab tests can show whether a sample of your sputum contains bacteria (such as the bacteria that cause tuberculosis) or fungi.
• Lung function tests. These tests measure how much air you can breathe in and out, how fast you can breathe air out, and how well your lungs deliver oxygen to your blood. Lung function tests help show how much lung damage you have.
• A sweat test or other tests for cystic fibrosis.
Bronchoscopy
If your bronchiectasis doesn't respond to treatment, your doctor may recommend bronchoscopy . Doctors use this procedure to look inside the airways.
During bronchoscopy, a flexible tube with a light on the end is inserted through your nose or mouth into your airways. The tube is called a bronchoscope. It provides a video image of your airways. You'll be given medicine to numb your upper airway and help you relax during the procedure. Bronchoscopy can show whether you have a blockage in your airways. The procedure also can show the source of any bleeding in your airways.
HOW IS BRONCHIECTASIS TREATED?
Bronchiectasis often is treated with medicines, hydration, and chest physical therapy (CPT). Your doctor may recommend surgery if the bronchiectasis is isolated to a section of lung or you have a lot of bleeding.
If the bronchiectasis is widespread and causing respiratory failure, your doctor may recommend oxygen therapy.
The goals of treatment are to:
• Treat any underlying conditions and lung infections.
• Remove mucus (a slimy substance) from your lungs. Maintaining good hydration helps with mucus removal.
• Prevent complications.
Early diagnosis and treatment of the underlying cause of bronchiectasis may help prevent further lung damage.
In addition, any disease associated with the bronchiectasis, such as cystic fibrosis or immunodeficiency, also should be treated.
Medicines
Your doctor may prescribe antibiotics, bronchodilators, expectorants, or mucus-thinning medicines to treat bronchiectasis.
Antibiotics
Antibiotics are the main treatment for the repeated lung infections that bronchiectasis causes. Oral antibiotics often are used to treat these infections.
For hard-to-treat infections, your doctor may prescribe intravenous (IV) antibiotics. These medicines are given through an IV line inserted into your arm. Your doctor may help you arrange for a home care provider to give you IV antibiotics at home.
Expectorants and Mucus-Thinning Medicines
Your doctor may prescribe expectorants and mucus thinners to help you cough up mucus.
Expectorants help loosen the mucus in your lungs. They often are combined with decongestants, which may provide extra relief. Mucus thinners, such as acetylcysteine, loosen the mucus to make it easier to cough up.
For some of these treatments, little information is available to show how well they work.
Hydration
Drinking plenty of fluid, especially water, helps prevent airway mucus from becoming thick and sticky. Good hydration helps keep airway mucus moist and slippery, which makes it easier to cough up.
Chest Physio Therapy/ Postural Drainage
CPT also is called physiotherapy (FIZ-e-o-THER-ah-pe) or chest clapping or percussion. This technique is generally performed by a respiratory therapist but can be done by a trained member of the family. It involves the therapist pounding your chest and back over and over with his or her hands or a device. Doing this helps loosen the mucus from your lungs so you can cough it up.
You can sit with your head tilted down or lie on your stomach with your head down while you do CPT. Gravity and force help drain the mucus from your lungs.
Some people find CPT hard or uncomfortable to do. Several devices can help with CPT, such as:
• An electric chest clapper, known as a mechanical percussor.
• An inflatable therapy vest that uses high-frequency air waves to force mucus toward your upper airways so you can cough it up.
• A small handheld device that you breathe out through. It causes vibrations that dislodge the mucus.
• A mask that creates vibrations to help break loose mucus from your airway walls.
Some of these methods and devices are popular with patients and doctors, but little information is available on how well they actually work. Choice usually is based on convenience and cost.
Several breathing techniques also are used to help move mucus to the upper airway so it can be coughed up. These techniques include forced expiration technique (FET) and active cycle breathing (ACB).
FET involves forcing out a couple of breaths and then doing relaxed breathing. ACB is FET that involves deep breathing exercises.
Other Treatments
Depending on your condition, your doctor also may recommend bronchodilators, inhaled corticosteroids, oxygen therapy, or surgery.
Bronchodilators
Bronchodilators relax the muscles around your airways. This helps open your airways and makes breathing easier. Most bronchodilators are inhaled medicines. You will use an inhaler or a nebulizer to breathe in a fine mist of medicine.
Inhaled bronchodilators work quickly because the medicine goes straight to your lungs. Your doctor may recommend that you use a bronchodilator right before you do CPT.
Inhaled Corticosteroids
If you also have wheezing or asthma with your bronchiectasis, your doctor may prescribe inhaled corticosteroids (used to treat inflammation in the airways).
Oxygen Therapy
Oxygen therapy can help raise low blood oxygen levels. For this treatment, you'll receive oxygen through nasal prongs or a mask. Oxygen therapy can be done at home, in a hospital, or in another health facility. (For more information, go to the Health Topics Oxygen Therapy article.)
Surgery
Your doctor may recommend surgery if no other treatments have helped and only one part of your airway is affected. If you have major bleeding in your airway, your doctor may recommend surgery to remove part of your airway or a procedure to control the bleeding.
In very rare instances of severe bronchiectasis, your doctor may recommend that you receive a lung transplant replacing your diseased lungs with a healthy set of lungs.
HOW CAN BRONCHIECTASIS BE PREVENTED?
To prevent bronchiectasis, it's important to prevent the lung infections and lung damage that can cause it.
Childhood vaccines for measles and whooping cough prevent infections related to these illnesses. These vaccines also reduce complications from these infections, such as bronchiectasis.
Avoiding toxic fumes, gases, smoke, and other harmful substances also can help protect your lungs.
Proper treatment of lung infections in children also may help preserve lung function and prevent lung damage that can lead to bronchiectasis.
Stay alert to keep children (and adults) from inhaling small objects (such as pieces of toys and food that might stick in a small airway). If you think you, your child, or someone else has inhaled a small object, seek prompt medical care.
In some cases, treating the underlying cause of bronchiectasis can slow or prevent its progression.
References:
http://www.nhlbi.nih.gov/
http://en.wikipedia.org/wiki/Bronchiectasis
http://www.uptodate.com/contents/clinical-manifestations-and-diagnosis-of-bronchiectasis-in-adults







